Hospice Volunteer and Wife Advocates Early Care
Published on February 16, 2022
Husband's hospice care supported family
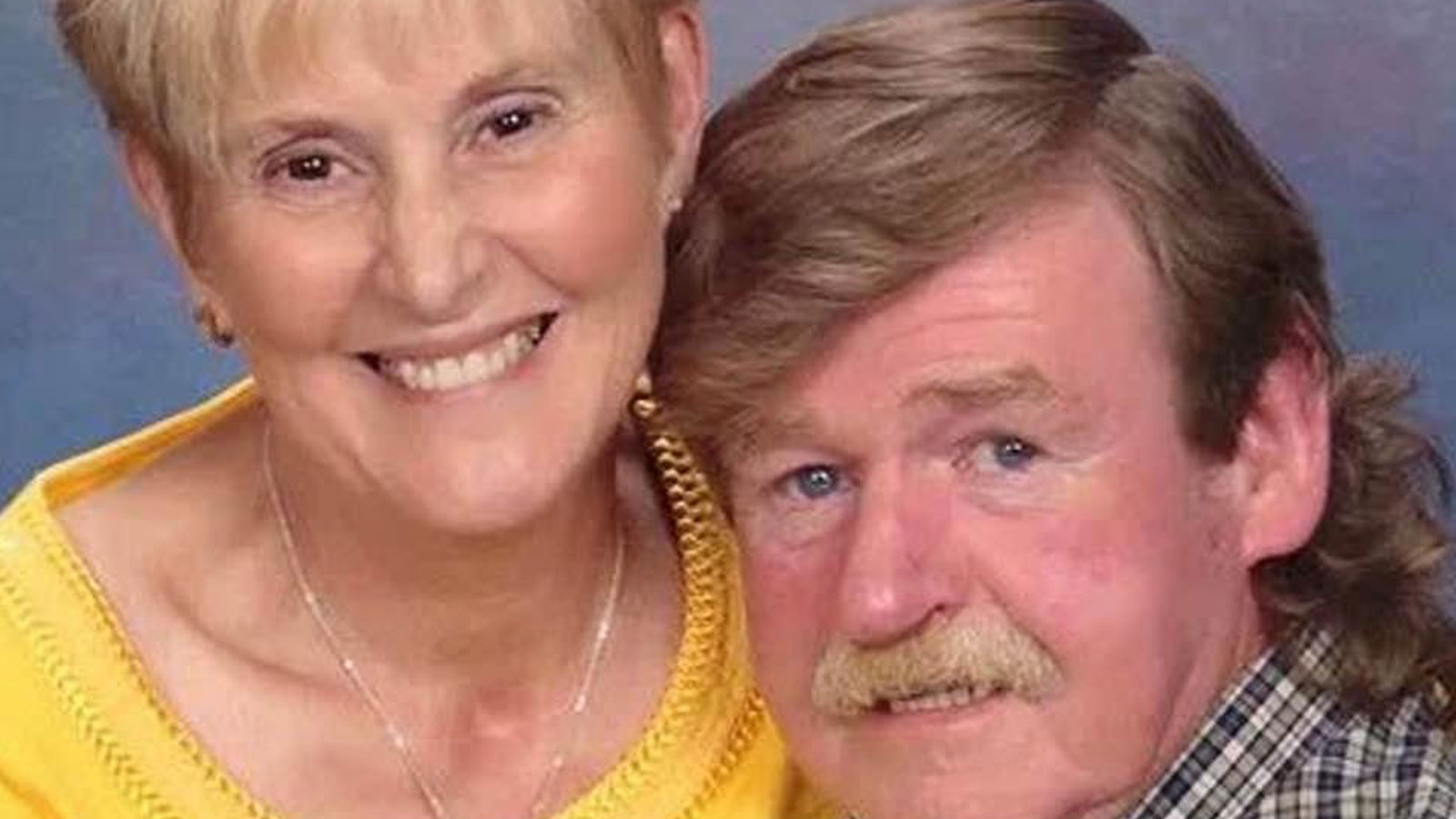
Lena Deter spent fifty-one years caring for others during her career as a nurse. When her own fit and active husband was unexpectedly diagnosed with late-stage mesothelioma at 70 years old, she knew she wanted the support of hospice for him…and for herself. Lena has been a volunteer with Alive for more than seven years. We spoke with her to learn more about how she got involved and how hospice care allowed her and her husband to spend their final days together, the way they wanted to.
How did you get involved with hospice?
I moved to Nashville and joined Cornerstone Church in 2012. I knew that I would be retiring and was looking for an opportunity to serve others.
During my nursing career, I worked in many different areas of nursing including radiation oncology and home health care within the Central Massachusetts area. Both of these specialties provided me with the honor of working with families and patients with complex medical issues and terminal illnesses. There was no hospice component at Cornerstone, but there I met Pastor Deeanna Wall who oversaw its hospital ministry. She connected me to Alive employees who attended Cornerstone. That led to my volunteering at Alive. I visited patients at home and in facilities, participated in focus groups, provided feedback on curriculum development, and participated in community outreach especially in advance care planning.
What was your personal experience with hospice?
Fast forward to the Monday before Thanksgiving in 2019.
My husband John underwent an annual diagnostic screening. That screening showed a significant change from the previous screening in November 2018. This led to multiple biopsies, healthcare provider visits, additional diagnostic testing, and a final diagnosis of stage four sarcomatoid mesothelioma, rare and incurable. It was a huge shock. John was alert, physically fit, and totally oriented. He interviewed hospices to find the best fit. Although I was volunteering with Alive for years by then, the choice needed to be his. In the end, he chose Alive.
The admitting nurse who met with him was a young veteran. John was retired military, and they hit it off. Everybody was phenomenal but having this nurse who understood his military service was critical. To connect with people really changes their care.
“Most people don’t enter hospice early enough. They don’t understand that pain management is different or that hospice can provide special equipment. They don’t understand the holistic approach of hospice. They don’t understand it’s about the best of quality of life. My husband went in because he wanted quality of life. I couldn’t imagine having someone I dearly love die without it.”
How do you know it’s time for hospice?
I knew John might not get the 6-12 months the doctor predicted and getting into hospice early was essential. People don’t realize they can leave hospice or stay longer than 6 months. Most people don’t enter hospice early enough. They don’t understand that pain management is different or that hospice can provide special equipment. They don’t understand the holistic approach of hospice. They don’t understand it’s about the best quality of life. My husband went in because he wanted quality of life. I couldn’t imagine having someone I dearly love die without it.
How did Alive personalize your hospice care?
John wanted to die at home in our bed and spend every moment he could with us. He wanted to finish the bathroom he was renovating. His goal was to live six months. He actually lived 46 days from the day of diagnosis. He died on a Sunday. That Monday before he was still putting up towel racks, cleaning out the shed, etc. He didn’t want a hospital bed, so we would lift him in and out of bed. Each morning, he got up and dressed every day at 6 A.M. He went to bed at 10 P.M. every night
Alive’s staff took time to get to know him. Everyone made sure to sit down and talk to him. He could get obnoxious at times, but they were just really good with him. They loved on him, and if he said, “No,” to something, the discussion was over. We had one nurse he didn’t gel with, so she didn’t return. The team listened to him and reassured him it was going to be his way no matter what.
 How did hospice support you after John’s death? How do you cope with grief?
How did hospice support you after John’s death? How do you cope with grief?
John died in 2020 right before COVID and the lockdown. It was really hard because of the lockdown. My daughter had zoom counseling sessions. My grandson was 11 when John died and has received virtual counseling also. For the first anniversary of his death, my sister and I did a memorial in the Grief Center. My sister flew in from Connecticut to be here with me for it. I continue monthly in-person grief counseling with Alive and run a grief ministry at my church to support others going through it too.
I was 19 and John was 22 when we married. It was a really great 48 years. We had come to such a phenomenal place. We had grown and changed so much, and in the last decade, we had become one. If we had just known at 40 what we know at 60! As two individuals, you struggle to maintain that before you learn the blessing of melding into one, which makes it so special. I wouldn’t give it up for the world. Even in the loss, it’s a fabulous thing that you carry.
“Having been on both sides, as a nurse and then as a wife, I really want people to know the benefits and ask the right questions of their healthcare providers.”
What do you want others to know about hospice?
There is so much misinformation, it breaks my heart. Some of it comes from doctors and nurses who don’t know hospice and don’t understand. Having been on both sides, as a nurse and then as a wife, I really want people to know the benefits and ask the right questions of their healthcare providers. You have a right to get multiple medical opinions and interview your healthcare providers. Ask questions. You have a right to refuse unwanted treatment. You have a right to die the way you want to.
Make your own advance directive here.
Click here to volunteer with Alive!